The aim of this multicentric study was to compare outcomes of waterjet ablation therapy (WAT) vs urethral-sparing robot assisted simple prostatectomy (usRASP) for large prostate volumes (>80ml) with regard to BPH6 (adequate relief from LUTS, high-quality recovery experience, maintenance of erectile and ejaculatory function, maintenance of continence, and avoidance of high-grade complications).
Three institutional BPH datasets (n=205) were matched and queried for “prostate volume>80 mL” (n=86), “WAT” (Group A; n=42) and “usRASP” (Group B; n=44). Baseline, perioperative and functional data according to BPH6 composite endpoint (symptom relief, quality of recovery, erectile function preservation, ejaculatory function preservation, continence preservation, and absence of major perioperative complications) were compared between groups. Differences between continuous variables were assessed with Kruskal-Wallis test, while Pearson’s χ2 test was used for categorical data. For all analyses, a two-sided p<0.05 was considered significant.
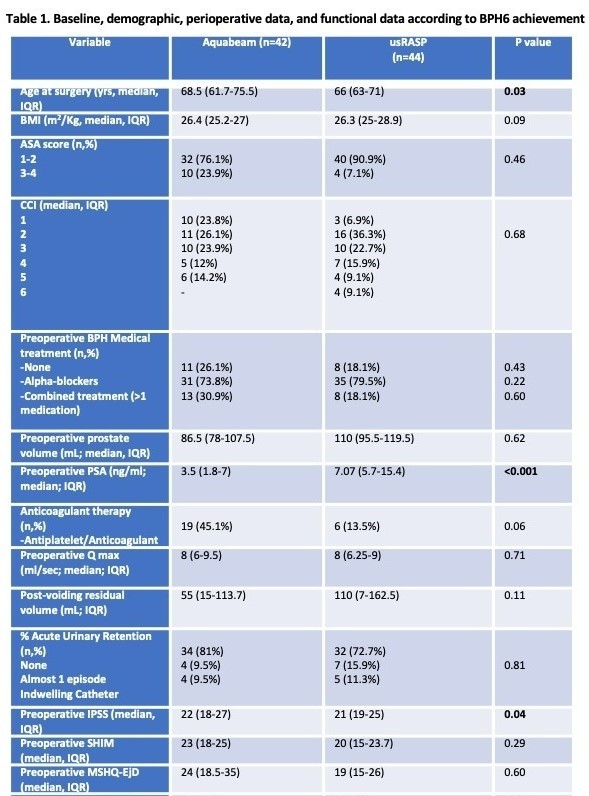
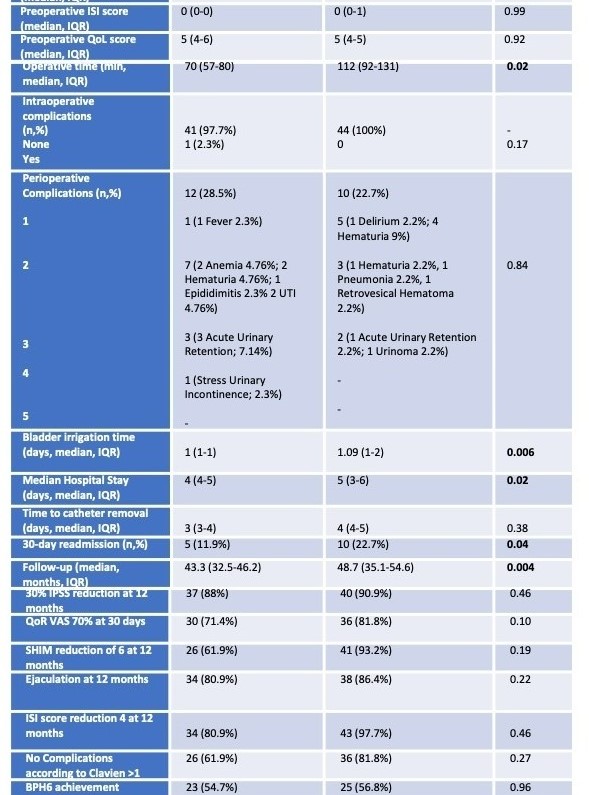
Baseline and perioperative data are reported in Table 1. Compared to group B, patients treated with WAT showed increased median age surgery (p=0.03), preoperative median IPSS (p=0.04) and lower preoperative PSA median values (p<0.001). All other baseline variables were comparable between groups (all p≥0.06; Table 1). Regarding perioperative outcomes, patients treated with usRASP revealed increased median operative time (p=0.02), prolonged bladder irrigation time (p=0.006), longer median hospital stay (p=0.02) increased 30-days readmission rate (p=0.04) and a longer follow-up timeframe(p=0.004). At a median follow-up of 43.7 months (IQR 33.8-49.7) the BPH6 achievement rate was comparable between groups (A:54.7% vs B:56.8%; p=0.96) with no significative difference between any of the domains considered (all p≥0.1, Table 1).
Compared to usRASP, WAT showed non-inferior symptom relief and ejaculatory function preservation for prostate gland>80 mL with a moderate benefit in terms of main perioperative outcomes at mid-term follow-up. Long-term outcomes of both procedures’ durability as standardized head-to-head comparisons with other novel technologies for BPH surgery are eagerly awaited in the upcoming future.