Hypothesis / aims of study
Artificial urinary sphincter (AUS) implantation has been the standard of care for male stress urinary incontinence (SUI) refractory to conservative treatment. Other devices are increasingly used. There are no clear recommendations on the patient characteristics that determine the best treatment option for male SUI. Therefore, EAU Research Foundation has initiated the prospective registry SATURN (Surgery for mAle incontinence with arTificial Urinary sphincters and slings). The reason for a registry as compared to an RCT is that for surgical treatments it is easier to attain equipoise. The objectives of the registry are to assess efficacy of male SUI surgery in daily life practice.
Study design, materials and methods
SATURN aims to analyze 1000 patients undergoing male SUI surgery with 10 year follow-up. Inclusion is closed (n=1000, 29 implanting centers in 9 European countries). Absence of pad use or only 1 security pad are considered “cured”. Patient related outcome measures (quality of life EQ-5D-5L, incontinence ICIQ-UI-SF) and data regarding complications are collected at baseline, around surgery, after 6 weeks (for devices that require activation), 12 weeks and yearly thereafter.
This abstract concerns data of the initial 500 patients who reached one year follow up.
Results
Twenty centers included 500 patients. Mean age was 69 (SD 8.1) years. Mean age, age adjusted Charlson Comorbidity Index score and BMI didn’t differ significantly per implant type.
Patients were suffering from incontinence after radical prostatectomy in 88% of whom 48% underwent a robot assisted laparoscopic prostatectomy. Radiotherapy (primary or salvage) was applied in 31% of all patients.
Preoperative urodynamic investigation was done in 67%, showing mainly pure SUI in 77% and mixed incontinence in 22%. Pure urgency incontinence and a hypocontractile detrusor were noticed in one patient. Cystoscopy preoperatively was performed in 92% of patients.
Devices implanted were: 332 AMS800, 85 Advance XP, 24 ATOMS, 21 VICTO (plus), 18 ProACT, 12 Argus, 3 ZSI375, 3 Virtue, 1 Remeex and 1 TILOOP. Of these patients 76% didn’t have a surgical previous treatment for SUI before the device implant that was registered into SATURN, 17% underwent one surgical previous treatment and 6% had two or more previous surgical treatments.
Pre-operative application of antibiotics, shaving or antiseptic washing at home were applied in respectively 7%, 25% and 12%. Perioperative antibiotics were administered in 98%. Shaving was done in the OR in 65% of patients.
A transurethral catheter was inserted in 79% and a suprapubic catheter in 12%. Nine percent of patients didn’t get a catheter. If a transurethral catheter was used, this was removed within 24 hours after surgery in 61%. In case of a suprapubic catheter this was done in 74%.
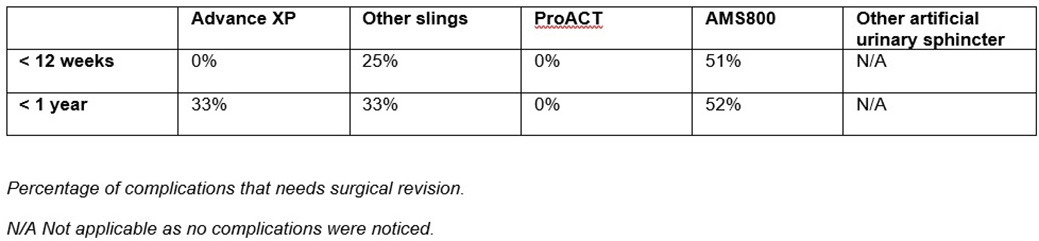
Complications during the first 12 postoperative weeks occurred mainly in AMS800, including mechanical failure, mispositioning of components, erosion, infection and retention. Whereas other devices reported much lower complication rates up to one year follow up. Surgical revision rates of complications are shown in Table 1.
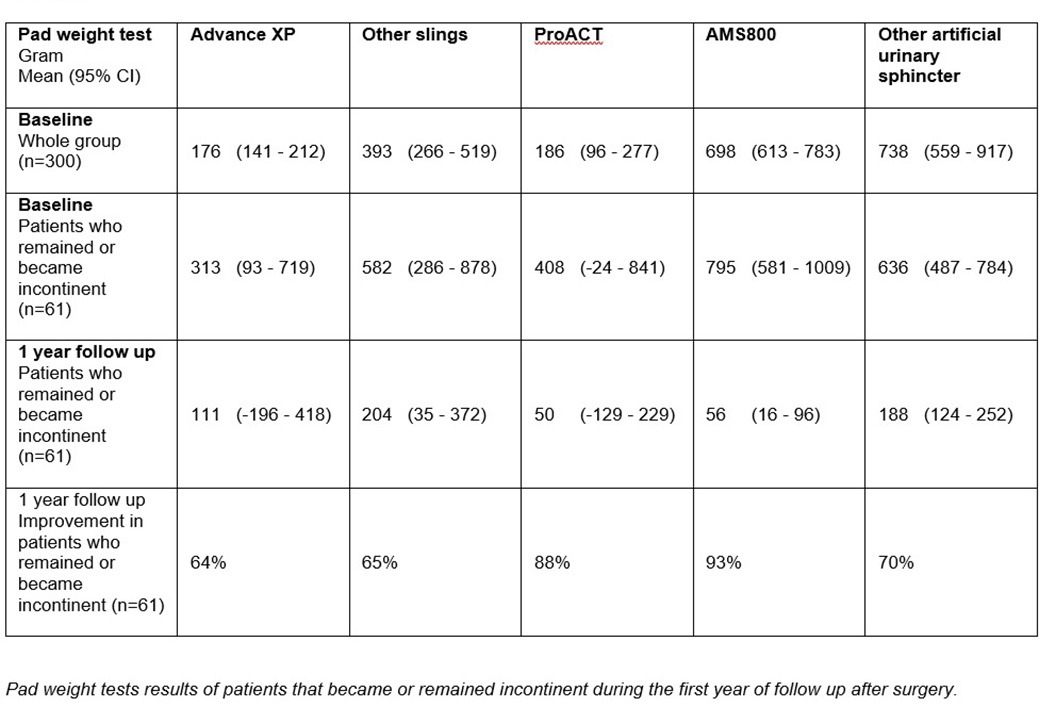
Cure rate for all devices at one year was 63% (n=400). Particularly in the ProACT group the increase in number of patients that became continent between 12 weeks and one year follow up was high (56%) as the device needs a period of outpatient adjustments before continence is reached. The majority of patients receiving other devices reached continence and remained so from the beginning. Eleven percent of all patients became incontinent again within one year, whereas 27% never became dry. Table 2 shows the pad weights at baseline before device implant surgery and at one year follow-up of the patients who became incontinent again or remained incontinent throughout the first year follow-up (n=147).
Interpretation of results
To our view a registry better reflects routine clinical practice than a RCT. The drawback of SATURN is that results need to be interpreted more carefully, as SATURN is not a randomized clinical trial. Data are generally not suitable for statistical analysis or direct comparison between implants on clinical outcomes, for example results of implanted devices that are only done in a few participating centers. Moreover, not all centers included patients at an even rate, which means that a learning curves, availability of alternatives and other results are biased by center specific influences.
Despite these limitations, SATURN registry provides us an opportunity to get a better insight in daily clinical practice of these devices.
Patients were suffering from prostatectomy for prostate cancer in 88%. Radiotherapy (primary or salvage) was applied in 31% of all patients. However, only in 5% radiotherapy was the main cause of stress urinary incontinence.
Preoperatively, we do not know how many patients were withheld from surgery based on urodynamics as patients were included if they went for surgery. Therefore from this registry , we cannot deduct whether urodynamic outcome defines the type of chosen device. Moreover, SATURN doesn’t give us the final answer about the necessity of performing urodynamics in males with SUI opting for surgery.
Complication rates need to be interpreted carefully as specific asked complications in SATURN refer more to AMS800 and other complications might be underreported. The high amount of AMS800 as compared to other devices may cause bias. Selection of device type is not randomized, but based on patient and/or surgeon preference. For example, in 300 patients the result of the pre-operative 24-hour pad test performed was higher for AMS800 as compared to the other alternatives. So, more severe incontinence is treated with a more voluminous device, which is consequently most likely more prone to complications. If a complication occurred, it was more likely to be approached surgically in patients with an AMS800 (Table 1).
As mentioned, preoperative 24-hours pad weight test was significantly higher for the AMS800 compared to other devices. However, if patients remained incontinent or noticed incontinence again after a postoperative period of continence, the remaining mean pad weight was relatively low (Table 2).
Concluding message
The first results of the SATURN registry in male stress urinary incontinence provide an impression of daily clinical practice and performance of implant devices. Longer follow up in a higher number of patients are into progress as the registry is still running.