Introduction
Lower urinary tract symptoms due to benign prostatic enlargement are a significant detractor from quality of life in aging men. Robotic assisted simple prostatectomy (RASP) and Thulium Laser Enucleation of the Prostate (ThuLEP) have both demonstrated improved outcomes compared to open simple prostatectomy for significantly enlarged prostates. We aim to compare the peri-operative and short-term outcomes of these newer procedures in patients with large (>80 gram) prostates.
Methods
A multi-institutional retrospective database of 120 consecutive RASPs performed by 2 expert robotic surgeons and 392 ThuLEPs performed by 4 expert surgeons were compared. Patient characteristics, peri-operative data, and patient outcomes (change in PSA, prostate tissue yield, incidence of stress urinary incontinence (SUI), and change in IPSS) were evaluated. Propensity score matching was performed for age, prostate size and PSA. Student&[prime]s T-Test and Chi squared were used for statistical comparison (p < 0.05).
Results
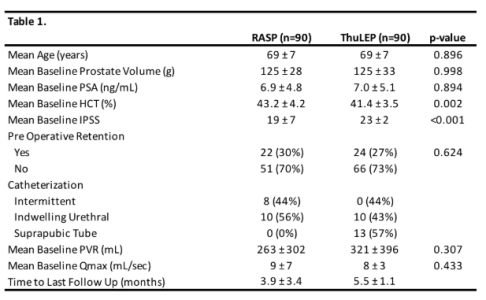
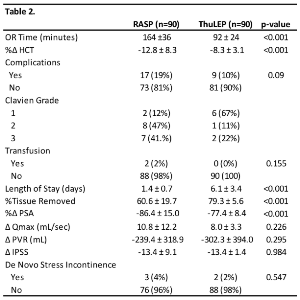
After matching for age, prostate size, and PSA, 90 patients were eligible for analysis in each group. Table 1 shows the baseline characteristics with noted differences in HCT (p=0.002) and IPSS ( < 0.001). Mean follow-up was 3.9 ± 3.4 months for RASP and 5.5 ± 1.0 months for ThuLEP. RASP demonstrated a significantly larger PSA reduction, while ThuLEP demonstrated a shorter OR time and larger percentage tissue yield (Table 2). Overall, functional outcomes were excellent in both groups. There was no significant difference in post-operative urinary parameters, IPSS change or de novo SUI between groups.
Conclusions
RASP and ThuLEP are both excellent options for symptomatic patients with significantly enlarged prostates. While RASP demonstrated a longer operative time and a greater drop in HCT, there was no difference in transfusion rates or functional outcomes. The discrepancy between tissue yield and PSA reduction requires further investigation.