Hypothesis / Aims of study
Sacral neuromodulation (SNM) is often applied for drug refractory overactive bladder (OAB), The effect of SNM on nycturia is unknown. SNM is superior to standard medical treatment and combination of SNM with antimuscarinics is more effective than antimuscarinics alone. [1] Different studies are consistent that about 70-75% of OAB patients have a >50% symptomatic improvement after SNM. [2] Moreover, significant reduction has been shown in the number of incontinence episodes (P < 0.0001) and the number of pads used (P < 0.0001) with marked improvement in quality of life after SNM therapy. The effect of SNM on Nocturia has not been studied. The aim of our study was to study the effect of SNM on nocturia episodes
Study design, materials and methods
TheTined Lead procedure (TLP) is used to test the neural integrity, therefore sensory and motor responses should be obtained during this test. The motor responses are important to identify the correct sacral root. Typical S3 stimulation results in bellows movement of the pelvic floor, plantar flexion of the great toe and paraesthesia in the rectum, perineum, scrotum, or vagina.
Stimulation of the other sacral roots results in different motor responses: S2 stimulation results in clamp movement or twisting and pinching of the anal sphincter and plantar flexion with lateral rotation of the entire foot; S4 stimulation results in bellows motion of the pelvic floor, no lower extremity activity and a sensation of pulling in the rectum. If the patient’s symptoms improve by at least 50% then the patient is a candidate to undergo the stage II or permanent step in which the permanent implantable pulse generator.
Sensation-related bladder diaries (SR-BDs) were assessed in all our patients who underwent SNM for idiopathic OAB between June 2016 and August 2018.
SNM was performed following a two-phased tined lead procedure under local or general anesthesia. The SR-BDs were collected prospectively.
Patients filled out a SR-BD, for 3 consecutive days at baseline and after 2 weeks, during a 4-week test phase. Bedtime and times of voiding, as well as intake were noted.
Results
A total of 40 (13 males, 27 females) patients with OAB, with and without incontinence (90 and 10% respectively), were included.
From these 40 patients, 26 had a successful test phase (>50% reduction of OAB symptoms). In patients with a successful test phase (T+), the number of nycturia episodes changed significantly from 1.7 ( ±1.6) to 1.1 (±1.3) P=0.009, while the mean volume voided at night remained the same (P=0.395).
The total number of voids frequency over 3 days was similar between baseline and during the test-phase (31 +/- 11 vs 30 +/- 5, P=0.297. There was no significant difference in fluid in intake prior versus during SNM test phase. There was no significant decrease in nycturia episodes in patients with a negative tined lead test, 1.1± 1.2 vs 1.9± 1.5 P=0.109. (< 50% reduction in OAB symptoms).
Interpretation of results
Based on a five-year prospective study by Van Kerrebroeck et al., one-year follow-up after surgery showed that treatment was effective in 84% of patients with urinary incontinence and 71% of urinary frequency-urgency patients, and at the end of a five-year follow-up period, these two indicators were 68 and 56%, respectively [3].
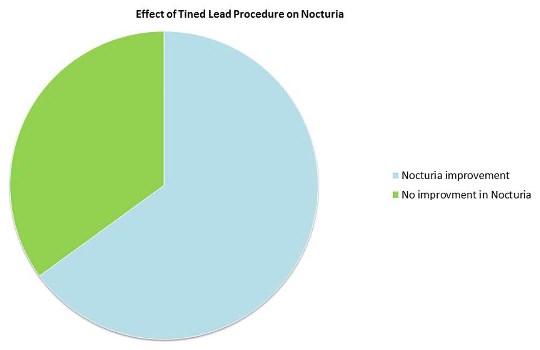
About 65% of patients included in our study showed a reduction of >50% of their OAB symptoms. In all these patients, nocturia was significantly reduced from about 2 to about 1 episode per night.
Concluding message
Nocturia is improved in about 65% of patients undergoing TLP for OAB who show a overall reduction of >50% of their OAB symptoms. These results show that SNM significantly modifies nycturia in patients with OAB, during a successful test phase a change in the mean volume voided at night.
Figure 1
References
Apostolidis A1, Averbeck MA2, Sahai A3, Rahnama’i MS4, Anding R5, Robinson D6, Gravas S7, Dmochowski R8. Can we create a valid treatment algorithm for patients with drug resistant overactive bladder (OAB) syndrome or detrusor overactivity (DO)? Results from a think tank (ICI-RS 2015). Neurourol Urodyn. 2017 Apr;36(4):882-893. doi: 10.1002/nau.23170.
Donon L, Robert G, Ballanger P. [Sacral neuromodulation: results of a monocentric study of 93 patients]. Prog Urol. 2014;24: 1120–1131.
van Kerrebroeck PE, van Voskuilen AC, Heesakkers JP et al. Results of SNM therapy for urinary voiding dysfunction: outcomes of a prospective, Worldwide Clinical Study. J Urol 2007;178:2029–2034
Disclosures
Funding none Clinical Trial No Subjects Human Ethics Committee MUMC Helsinki Yes Informed Consent Yes