Introduction and objective
Evaluating outcomes after benign prostate hyperplasia (BPH) surgery among men with lower urinary tract symptoms (LUTS) only versus those with urinary retention (UR)
Methods
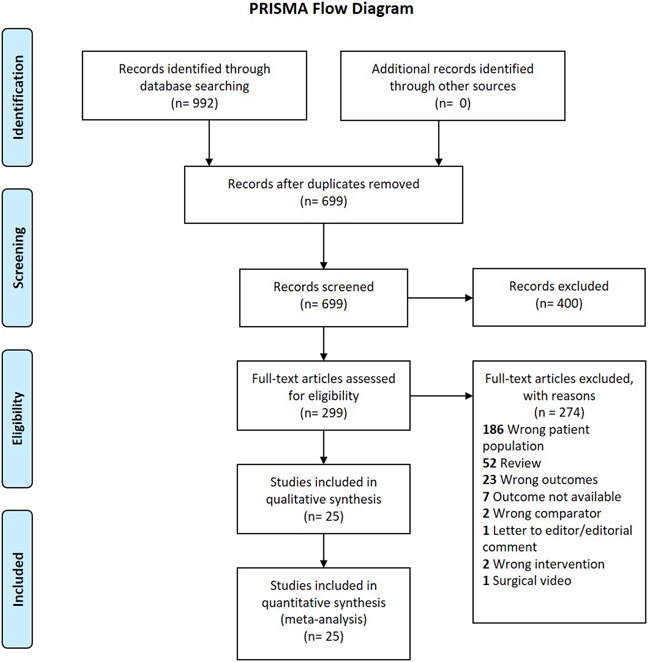
Eligible studies identified from four electronic databases. Search, data extraction and quality assessment were performed independently by two reviewers. Studies with perioperative, functional, early and late complication outcomes included.
Results
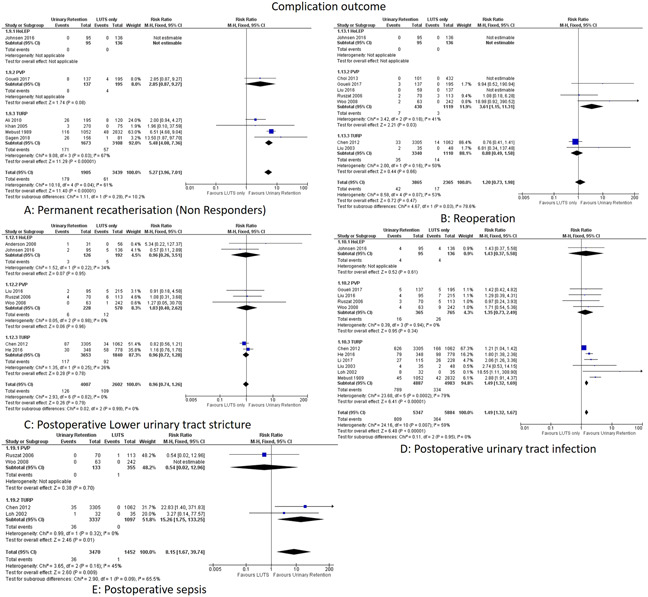
Twenty-five studies, 14,593 patients including 1 randomized controlled trial, 11 prospective and 13 retrospective studies included for meta-analysis. This showed higher risk of immediate transient re-catherization (Risk Ratio (RR): 5.29, p <0.00001), longer days to trial-off-catheter (mean difference (MD):0.25, p <0.00001), longer hospitalization stay in the urinary retention group (MD: 0.35, p <0.00001),and higher risk of intraoperative blood transfusions (RR: 1.90, p=0.002), post-operative urinary tract infections (RR: 1.49, p <0.00001) and sepsis (RR: 8.15, p=0.009) too. Failure of surgery like permanent re-catheterization (RR: 5.27, p <0.00001) was more in pre-operative UR group. Negligible differences seen in long term functional outcomes between the two groups (International Prostate Symptom Score at 12 months, MD: -0.06, p=0.68; Quality of Life at 12 months, MD: 0.20, p <0.00001; maximum urinary flow rate (Qmax) at 12 months, MD: -0.33, p=0.10; and post void residual volume at 12 months, MD: 4.32, p <0.00001)
Conclusions
Preoperative UR patients undergoing surgery for BPH have higher risk of post-operative complications versus LUTS only group including the need for permanent catheterisation. Both groups had similar long-term functional outcomes. We could infer that patients with UR on whom surgery is successful, with time may recover bladder function akin to patients with LUTS alone.
Source of Funding
N.A